Physician Credentialing Services: Get Enrolled Faster, Get Paid Sooner
You can deliver exceptional patient care, hire the best providers, and invest in advanced systems, but if your physicians aren’t properly credentialed, your revenue stops before it starts. Claims get denied, reimbursements are delayed, and practices lose months of income simply because credentialing wasn’t handled correctly or on time.
Physician credentialing is not just paperwork; it’s the gateway to getting paid.
That’s why Physician Credentialing Services from Bridge Billing Services are essential for providers, professionals, and hospitals looking to grow efficiently. Whether you’re opening a new practice, onboarding new physicians, expanding locations, or contracting with new payers, credentialing accuracy directly impacts your cash flow.
If you’re searching for reliable medical billing services, California medical billing services, or professional billing solutions for healthcare providers, this guide explains what physician credentialing is, why it matters, and how Bridge Billing Services helps you get enrolled faster and paid without disruption.
What Are Physician Credentialing Services and Why Are They Important?
Understanding Physician Credentialing
Physician credentialing is the process of verifying and enrolling healthcare providers with insurance companies, government programs, and healthcare organizations so they are authorized to bill and receive payment for services.
Credentialing verifies:
- Education and training
- Licensure and certifications
- Board status
- Work history
- Malpractice coverage
- DEA and NPI information
- Compliance with payer and regulatory standards
Once verified, the provider is enrolled with payers such as Medicare, Medi-Cal, and commercial insurance plans.
Why Physician Credentialing Is Critical
Without proper credentialing:
- Claims are denied or rejected
- Payments are delayed for months
- Practices lose revenue permanently
- Patient access is restricted
- Compliance risks increase
Credentialing is foundational to medical billing services and revenue cycle success, especially in California, where payer rules are complex and timelines are strict.
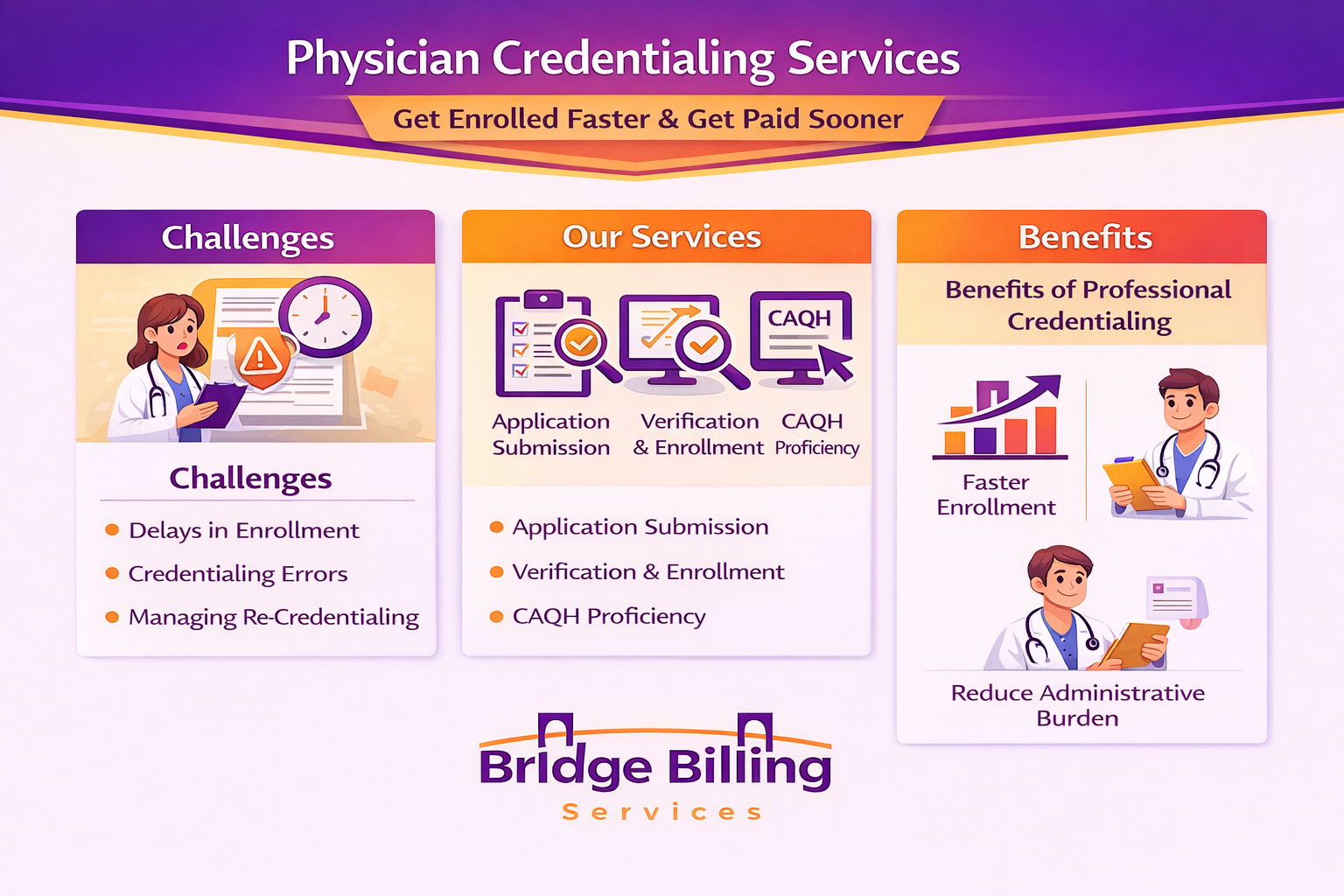
Why Physician Credentialing Is So Complex
Payer Rules, Timelines & Constant Updates
Credentialing is not a one-time task; it’s an ongoing process with frequent updates and revalidations.
Common credentialing challenges include:
- Long payer processing times (60–180 days)
- Incomplete or inconsistent applications
- CAQH profile errors
- Missed re-credentialing deadlines
- Changes in provider status or locations
- Multiple payers with different rules
- Medicare, Medi-Cal, and HMO variations
In California, additional complexity comes from IPAs, delegated entities, Medi-Cal managed care plans, and regional payers, making local expertise essential when choosing California billing services near me.
How Bridge Billing Services Supports Physician Credentialing
Professional Billing Solutions for Healthcare Providers in California & Nationwide
Bridge Billing Services delivers end-to-end Physician Credentialing Services that integrate seamlessly with medical billing and revenue cycle operations.
1. New Provider Credentialing & Enrollment
We manage the entire enrollment process for:
- Individual physicians
- Group practices
- Hospitals and clinics
- Multi-location organizations
From initial applications to final payer approval, we ensure nothing is missed.
2. Medicare, Medi-Cal & Commercial Payer Enrollment
Our team handles enrollment with:
- Medicare
- Medi-Cal
- Commercial insurance plans
- HMOs and PPOs
- IPAs and delegated entities
This ensures providers can bill without interruption.
3. CAQH Profile Setup & Maintenance
CAQH errors are a leading cause of credentialing delays. We:
- Create and update CAQH profiles
- Ensure accuracy and completeness
- Monitor attestations and revalidations
4. Re-Credentialing & Ongoing Maintenance
Credentialing doesn’t stop after approval. Bridge Billing Services manages:
- Re-credentialing cycles
- License renewals
- Insurance updates
- Location and ownership changes
This prevents silent payer terminations.
5. Integration With Medical Billing Services
Because credentialing and billing are tightly linked, our credentialing services work hand-in-hand with our outsourced medical billing California solutions, ensuring claims are submitted correctly from day one.
All workflows are secure and fully compliant, supporting HIPAA-compliant medical billing services nationwide.
Why Outsourcing Physician Credentialing Improves Revenue
Outsourced Medical Billing California Advantage
Many practices outsource credentialing because:
- In-house staff lack payer-specific expertise
- Credentialing delays stall billing
- Missed deadlines cause revenue loss
- Growth requires scalable processes
With outsourced credentialing from Bridge Billing Services, providers gain:
- Faster payer enrollment
- Fewer denials due to credentialing issues
- Reduced administrative burden
- Improved cash flow
- Full visibility into credentialing status
This is why providers searching for a dependable medical billing company near me often choose a partner that offers both billing and credentialing expertise.
Bridge Billing Services Tips for Successful Credentialing
- Start credentialing early before provider start dates
- Keep CAQH profiles updated at all times
- Track re-credentialing deadlines proactively
- Notify payers immediately of provider changes
- Align credentialing with billing workflows
- Partner with credentialing specialists, not generalists
These best practices are built into every Bridge Billing Services credentialing workflow.
Neighborhoods We Serve
Bridge Billing Services proudly supports providers and healthcare organizations in:
- Los Angeles
- Orange County
- San Diego
- Riverside
- San Bernardino
- Sacramento
- San Francisco Bay Area
- Fresno & Central Valley
And providers across all 50 states.
Physician Credentialling Services
Physician credentialing is not optional; it’s the foundation of your revenue cycle. Delays, errors, or missed deadlines can cost practices thousands in lost reimbursement. With the right partner, credentialing becomes a strategic advantage instead of a bottleneck.
Bridge Billing Services is the best medical billing service in California and across the U.S., providing expert physician credentialing services that accelerate enrollment, protect revenue, and support long-term growth.
Ready to get credentialed faster and paid without delays? Partner with Bridge Billing Services today.
FAQs
- What are physician credentialing services?
Services that verify provider qualifications and enroll them with insurance payers. - Why is physician credentialing important?
Without it, providers cannot bill or receive insurance payments. - How long does physician credentialing take?
Typically 60–180 days, depending on the payer. - Does Bridge Billing Services handle Medicare and Medi-Cal credentialing?
Yes, including managed care plans. - What is CAQH, and why is it important?
CAQH is a centralized provider database used by many insurers for credentialing. - Can credentialing delays affect billing?
Yes, claims will be denied if providers are not credentialed. - Do you manage re-credentialing?
Yes, including renewals and ongoing maintenance. - Can you credential multi-location practices?
Absolutely, we support practices of all sizes. - Is credentialing HIPAA compliant?
Yes, when managed by Bridge Billing Services. - Do you provide nationwide credentialing services?
Yes, across California and the U.S.